1. Sleep Testing
An objective evaluation of your sleep is needed before your board-certified, sleep physician can make a diagnosis. Options include:

In-lab overnight sleep study
This type of sleep study requires you to stay overnight at a sleep center, in a room that may resemble a hotel room. You will sleep with sensors hooked up to various parts of your body. These sensors record your brain waves, heartbeat, breathing and movement. Doctors usually recommend a sleep study for more complex cases.

Home sleep apnea test
Some patients with risk factors for obstructive sleep apnea may be candidates for a home sleep apnea test. This type of sleep study lets you sleep in the comfort of your own home while a small monitor collects data as you sleep. The testing equipment differs in that it is less complicated than what is used in an overnight sleep study. A sleep coordinator will show you how to use the testing equipment. Afterward, you take the device back to the sleep coordinator and the test is interpreted by a pulmonologist who makes the diagnosis. After your sleep study or home sleep apnea test, you will schedule a follow-up appointment to discuss the results.
2. Oral Appliance Therapy
What is an oral appliance and how does it work?
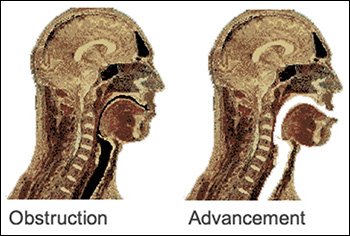
Mandibular (Lower Jaw) Advancement Devices (MAD)
Mandibular advancement devices are by far the most common type of dental sleep device available for the treatment of snoring and Obstructive Sleep Apnea (OSA). They are also sometimes called oral appliances, or dental sleep devices.

Mandibular Advancement Devices (MADs) open the airway by moving the mandible (the lower jaw) forward. The tongue is attached to the lower jaw behind the chin. As the jaw is moved forward, the collapsible part of your airway is held open by the forward movement of the tongue and other airway muscles. Mandibular Advancement Devices also improve the strength and rigidity of the airway by increasing the muscle activity of the tongue and other muscles of the airway.
3. PAP Therapy
Positive airway pressure (PAP) therapy
Positive airway pressure therapy treats Obstructive Sleep Apnea (OSA) by creating a “pneumatic splint” for the upper airway, PAP therapy prevents the soft tissues of the upper airway from narrowing and collapsing. Pressurized air is sent from a therapy device through air tubing and a mask to the upper airway.
Patients with severe sleep apnea are able to experience restful sleep with positive airway pressure therapy. Learn more about the types of PAP therapy below.
CPAP, APAP and BiPAP therapy
- Continuous positive airway pressure (CPAP): pressurized air at one fixed pressure
- Automatic positive airway pressure (APAP) therapy: automatically adjusted air levels based on a patient’s breathing (suited to patients with REM-related sleep apnea, positional apnea or those who are noncompliant with standard CPAP therapy)
- Bilevel therapy: higher inspiratory pressure and lower expiratory pressure (appropriate for certain patients who are non-compliant)
4. Alternative treatment options
Surgery is also an option for treating Obstructive Sleep Apnea (OSA), though it comes with associated risks and complications. Uvulopalatopharyngoplasty (UPPP), the most commonly performed surgical procedure for OSA in the United States, is effective in reducing snoring initially. Over the long term, UPPP cures snoring in 46% to 73% of patients who have had the surgery1.
1. Kashima ML (2007). Selected disorders of the nose and throat: Epistaxis, snoring, anosmia, hoarseness, and hiccups. In NH Fiebach et al., eds., Principles of Ambulatory Medicine, 7th ed., pp. 1849–1864. Philadelphia: Lippincott Williams and Wilkins.
5. Sleep Hygiene
Did you know there’s a term for your bedtime rituals and nightly habits? Collectively, these behaviors are known as sleep hygiene and they play an important role in a good night’s sleep.
The following link will provide guidelines for establishing good sleep hygiene: https://www.tuck.com/sleep-hygiene/